OVERVIEW YouTube Video Link: https://youtu.be/vWHjrjBx1cg
Method Selection
Published professional recommendations (e.g., ERS/ATS) address select methods for Bronchial Provocation testing1-5. Overall, these recommendations focus on the rationale, indications, and limitations/contraindications for each of the tests described. They are well defined, purposeful, and provide an abundance of supporting (evidence-based) published medical literature. However, what is lacking is a clear guidance regarding how to determine/select the appropriate method of bronchial provocation that is based upon the initial subject presentation.
So, as we get into this Focus Area, let’s consider the following scenario:
A 27 y.o. male (71”, 173 lb.) is referred to the Pulmonary Diagnostic Services to “Evaluate” as he experiences periodic, yet possibly increasing, episodes of an inability to “catch his breath”. His breathing difficulty often occurs when cutting certain types of wood (i.e., pine). The subject also states that he experiences this breathing discomfort when he begins jogging, but it often subsides after some time into his exercise routine.
The subject presents to the laboratory in no apparent distress and states that his breathing is currently “fine”. The subject’s PHM is unremarkable for cardiopulmonary disease, or other acute or chronic conditions. He has been an avid runner since high school (cross country team for 4 years). While still enjoying running, his current level of exercise is inconsistent (1-4 days/week), due to varying work shifts; he is employed as a laborer, in a wood processing plant.
Since the Pulmonary Diagnostic Services request for testing stated to “Evaluate” this subject, the Technologist Driven Protocol (TDP), “INDICATIONS-BASED PULMONARY DIAGNOSTICS: INITIAL SUBJECT EVALUATION” https://pftlabresources.com/tdp-indications-based-pulmonary-diagnostics-initial-subject-evaluation/ was employed to assess if there was evidence of airflow limitation. This TDP and others may be located in the RESOURCES Section of the Pulmonary Diagnostic Laboratory Resource Center @ www.pftlabreources.com .
Baseline pulmonary diagnostic studies (data and graphics not shown) did not indicate any gross abnormalities, as the values fell within the broad range of “normal”.
- Spirometry (Flow/Volume Loop) revealed no evidence of overt airflow limitation on exhalation and inhalation. However, the terminal portion of the forced exhalation suggested possible airflow slowing since the flow-volume curve was disproportionally reduced relative to the other portions of the expiratory curve. The PEF was greater than his reference range which may be due to either increased pulmonary elastic recoil, increased respiratory muscle strength, or both.
- Airway Mechanics revealed normal Raw and a slightly reduce sGaw which may represent peripheral airways dysfunction.
- Static Lung Volumes (via plethysmography) revealed no evidence of air-trapping. Unventilated lung studies were not performed during this visit since the plethysmograph derived data did not support this additional testing
- DLCOsb was not indicated during this session as the other studies were essentially within the normal limits. However, this test should be considered essential if there was a history associated with other types of dust exposure, e.g., asbestos.
- Resting Arterial Blood Gases were not performed. However, a resting, room air SpO2 was 98%; palpated and device HR were equivalent.
The next question would be, how would you proceed? And, more importantly, what did you base your decision upon?
According to the validated TDP that was utilized to determine which baseline studies would be most appropriate for this subject, the next step would be for a “Bronchial Provocation Study” to be performed. This seems reasonable since baseline studies, for the most part, landed within the “normal” range.
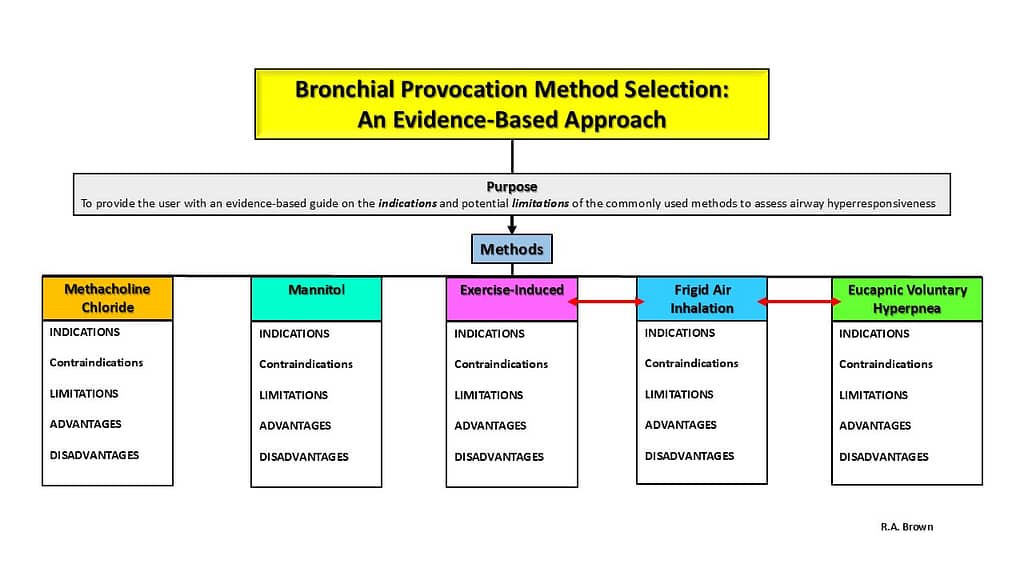
Here are your laboratory Bronchial Provocation options**: Methacholine Chloride Inhalation, Mannitol Inhalation, Exercise-Induced Bronchoconstriction (bicycle ergometer or treadmill), Frigid Air Inhalation, or Eucapnic Voluntary Hyperpnea.
Regarding this scenario, which option would you initially choose and (again) what evidence did you use to base your decision?
For example, within your practice you use Methacholine as the primary source for bronchial provocation testing. If you have other options available, why would you continue to do that? What evidence-based information do you have at your disposal to make a more informed decision? This is particularly important since not all individuals, with reactive airways disease, will have a positive response to Methacholine inhalation.6
As can be appreciated, this topic is multifactorial and therefore does not have a one size that fits all answer.
The following information will hopefully provide some level of insight/guidance on selecting the initial Bronchial Provocation Test Method for a given subject being evaluated for reactive airways dysfunction.
As always, please let me know if you have any constructive comments on how this section might be improved at https://pftlabresources.com/contact/ .
Cheers!
Bob
**Also, some additional Considerations for this topic:
·While being an important inducer for airway hyperresponsiveness, other than a brief review of the Mechanism of Action (MoA), Histamine challenge is not addressed in this presentation as it is used infrequently in the U.S., primarily due to the potential side-effects incurred with non-responsive individuals.
·Hyper- and/or Hypotonic aerosol administration is not commonly performed in the U.S. & these too will not be addressed
·Also, Environmental/Allergan challenge studies were not addressed since there are very few sites capable of providing prolonged subject observation; a positive response may take hours, to days, to months to be elicited.
Finally, major emphasis is placed upon the use of spirometric data to assess test response (e.g., FEV1). Forced spirometry is a well described protocol and, when performed according to published standards, can produce reproducible measures. However, spirometry is an insensitive tool and may not adequately detect bronchoconstriction in all symptomatic individuals. Therefore, I highly recommend checking out the Focus Area listed for “Airway Mechanics; Raw, Gaw, sRaw and sGaw” in the RESOURCES Section of the Pulmonary Diagnostic Laboratory Resource Center.
Supporting Literature:
- Coates AL, Wanger J, Cockcroft DW, Culver BH, Carlsen K-H, Diamant Z, Gauvreau G, Hall GL, Hallstrand TS, Horvath I, et al. ERS technical standard on bronchial challenge testing: general considerations and performance of methacholine challenge tests. Eur Respir J 2017;49:1601526.
- Procedure Name: Mannitol Challenge Test. ATS Pulmonary Function Laboratory Management and Procedure Manual, Third Edition 2016:141-149.
- Parsons JP, Hallstrand TS, Mastronarde JG, et al. An Official American Thoracic Society Clinical Practice Guideline: Exercise-induced Bronchoconstriction. Am J Respir Crit Care 2013: 187, 9, pp 1016–1027.
- Procedure Name: Methacholine Challenge Test. ATS Pulmonary Function Laboratory Management and Procedure Manual, Third Edition 2016:122-140a.
- Procedure Name: Exercise Challenge Test. ATS Pulmonary Function Laboratory Management and Procedure Manual, Third Edition 2016:150-168.
- Stocks J, Tripp M, Lin T. Methacholine challenge is insufficient to exclude bronchial hyper-responsiveness in a symptomatic military population. J Asthma 2014: 51;886-890.
Go to the video, “Bronchial Provocation Method Selection: An Evidence-Based Approach” at: https://youtu.be/bFoL_j9_eCQ